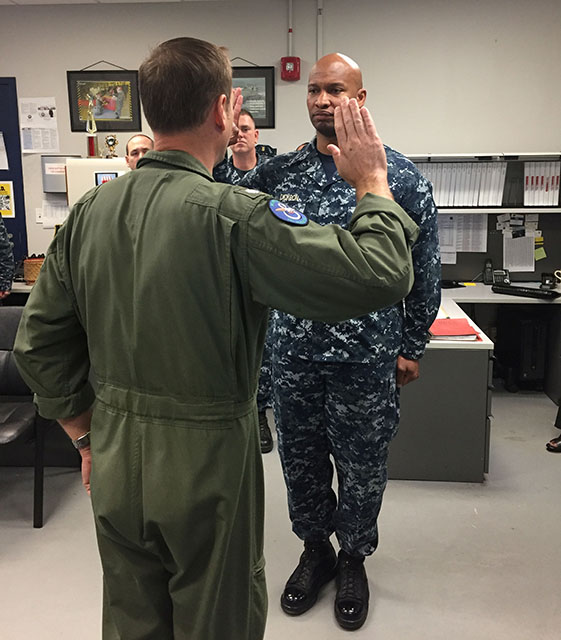
When I took my final oath as a Navy Chief Warrant Officer, I had no idea the most difficult part of service would come after I retired the uniform. For many veterans, the transition is quiet. But the battle doesn’t end. It shifts inward.
This commentary builds on that story and focuses on what happens after the transition, when the support offered falls behind the needs of those it’s meant to serve. It raises a new question:
Why is mental health still treated with pharmaceutical trial and error when brain technology could guide care from the beginning?
That question has been weighing heavily on me. Over the past month, I’ve spoken with veterans from all over the country, some quietly managing, others on the edge. Their experiences echo a common pattern: lingering fatigue, brain fog, emotional swings, and a quiet sense that something’s off, but no clear path forward. These aren’t abstract cases. They’re people I know. People like me. And like so many of us, they’ve been taught to push through rather than speak up.
But hitting a wall shouldn’t be the moment we start trying to figure out what’s wrong. And yet, that’s often when help finally arrives—after medications, side effects, and mounting frustration. There must be a better way.
Left of Bang: Anticipating the Crisis Before It Hits
In military terms, left of bang means identifying warning signs before a major event— the “bang”—occurs. On the battlefield, this saves lives. At home, it should protect wellness.
But far too often, our systems are set up to respond right of bang, when a veteran breaks down, ends up in the ER, or worse.
It’s costing lives.
In the year I retired, 2022, 6,407 U.S. veterans died by suicide. That’s 17.6 lives lost every single day1. Fathers. Mothers. Sons. Daughters. Teammates. The silence surrounding their pain is deafening.
Even more sobering, nearly 60% of those who died by suicide were not actively engaged in VA care at the time. Not because they didn’t want help, but because the system didn’t reach them in time, didn’t offer the right tools, or didn’t feel accessible.
Being Proactive Doesn’t Require a Crisis
We already know what saves lives: connection, awareness, and early support.
“Left of bang” in the context of mental health refers to normalizing check-ins and integrating brain wellness into our daily lives.
- It’s a buddy saying, “You’ve been on my mind. How are you really?”
- It’s a spouse asking, “Something seems off. Can we talk?”
- It’s a doctor screening for cognitive changes even during a routine visit.
- It’s a workplace offering support before someone reaches burnout.
These aren’t revolutionary ideas. They’re common-sense strategies rooted in one belief: The best time to act is before someone is in crisis.
Brain Health Is Readiness
In the military, we train our bodies to stay mission ready. But too often, we overlook the very thing that carries us through every challenge: the brain. It’s been our compass through uncertainty, stress, and loss. Yet, when it comes to care, mental health is still treated like a last resort, something reactive rather than essential.
That mindset has to change.
When we treat brain health as a pillar of performance—not just a response to pathology—we unlock a better path forward. Programs that utilize non-invasive technology, proactive assessments, and precision neuroregulation are already helping veterans restore and optimize brain function before it deteriorates.
And yet, many of our most outdated systems still require active-duty service members to “fail” prescription drug protocols before they can access advanced neuromodulation. In 2025, that’s more than archaic—it’s unacceptable.
We owe it to those who serve, and those who have served, to lead with better solutions, not wait for breakdowns.
This Is Personal
Before I became an advocate in this space, I was one of those veterans “pushing through.”
When I left the Navy, I had no idea how much was unraveling under the surface. I could still show up, still lead, still smile, so I assumed I was fine.
I wasn’t.
What helped wasn’t a crisis hotline. It was proactive, brain-focused care, accompanied by a supportive community. I didn’t need to prove I was broken to receive support; I needed to be seen early and treated like someone worth investing in from the start.
Healing isn’t something we earn after the fact. It’s something we’re all entitled to protect every single day.
Where Do We Go from Here?
With Mental Health Awareness Month approaching, this is our chance to transition from awareness to action.
Veterans don’t want pity, they want tools. They want to be seen early, not just when the pain becomes unmanageable. And they want to know that someone is fighting for their wellness before the battle becomes overwhelming.
So, here’s my call to action:
- If you’re a provider: Integrate brain health and cognitive screening into your intake—even if the issue isn’t obvious.
- If you’re a policymaker: Push for access to preventative brain-based care and remove outdated barriers to innovation.
- If you’re a family member, friend, or colleague: Check in early. Don’t wait for someone to “seem bad enough.” Ask for help!
- If you’re a veteran: You are not alone—and you don’t have to wait until you’re in crisis to seek help. There are options that work.
Let’s Keep the Conversation Going
Let’s make proactive care the norm, not the exception.
Let’s embrace innovation in brain health as part of readiness and long-term recovery.
Let’s stop waiting for a crisis.
What if prevention, not crisis, became the catalyst for care?
Reflection Questions to Keep the Dialogue Going
- Have you ever noticed signs of struggle—either in yourself or someone close to you—before things reached a breaking point? What did you do?
- What would “left of bang” support have looked like for you?
- Who showed up for you before you hit crisis, and what did that mean to you?
- If you could redesign veteran mental health support, where would you start?
- What does proactive care mean to you, and how do we make it the norm?
What if your brain had a baseline before life knocked it off course?
Your service may be behind you, but your mission continues. This time, it’s personal. This chapter isn’t just about recovery; it’s about reclaiming clarity, strength, and purpose. Healing isn’t weakness, it’s strategy. It’s leadership. And it starts before the breaking point.
Stay sharp, stay connected, and keep showing up—for yourself and for those still in the fight.
Because the path forward doesn’t begin at the bang.
It starts to the left of it.
- U.S. Department of Veterans Affairs, 2024 National Veteran Suicide Prevention Annual Report
https://www.mentalhealth.va.gov/suicide_prevention/data.asp
