A New Approach to Treatment of Traumatic Brain Injury and Concussions
Long-term adverse effects can be addressed with MeRT or Magnetic e-Resonance Therapy.

Simply stated, we use a magnetic field to stimulate, balance, and restore brain function, guided by very sophisticated imaging and diagnostics.
MeRT Approach
Concussion and Traumatic Brain Injury

Traumatic brain injuries and concussions are common in athletes who may experience multiple “head hits.” These hits affect the brain, and over time, the damage becomes cumulative. Members of the military are also commonly affected, but TBIs or concussions can happen to anyone.
Those who have suffered a traumatic brain injury may need other therapies to assist with regaining memory, learning skills, coordination, physical function, speech, and coping mechanisms. Brain injuries are complex and can affect many aspects of a person’s life, including their emotions and the ability to think clearly.
The CDC (Centers for Disease Control) defines a traumatic brain injury (TBI) as:
A blow to the head or a penetrating head injury that disrupts the normal function of the brain. TBI can result when the head suddenly and violently hits an object or when an object pierces the skull and enters brain tissue. An injury can also occur without a direct blow to the head, such as in an auto accident where the forces cause the head to move violently in one direction and then snap back in another direction.
This causes the brain to be jostled around inside the skull and can also injure the brain. Suffering a closed head injury can produce symptoms that range from mild to severe, based on the degree of damage that was done to the brain. While it’s possible for a person to experience a TBI to not have a loss of consciousness, in moderate to severe cases, LOC does usually happen. More severe cases of traumatic brain injuries often can result in coma or even death.”
Call Our New Patient Coordinator to Learn More
(619) 255-2101
Or fill in the form below and she will contact you.
Causes of TBI include:
- Falls (especially in older adults and young children)
- Motor vehicle crashes and other transportation-related causes (eg, bicycle crashes, collisions with pedestrians)
- Assaults
- Sports activities (eg, sports-related concussions)
 Symptoms of a Concussion or Traumatic Brain Injury
Symptoms of a Concussion or Traumatic Brain Injury
Depending on the severity of the injury, symptoms can include:
- Loss of consciousness
- Headaches or Migraines
- Fatigue or lethargy
- Vision changes and/or dilated pupils
- Dizziness or lightheadedness
- Memory issues
- Confusion
- Cognitive problems or decline
- Inappropriate emotional responses
- Anger
- Depression
- Anxiety or panic attacks
- Feeling of isolation
- Post-Traumatic Stress Disorder (PTSD)
- Numbness and tingling in different parts of the body
- Facial weakness
- Loss of function or weakness in other parts of the body
- Loss of bladder or bowel control
- Breathing problems
- Loss of hearing or tinnitus
 An Entirely New Approach
An Entirely New Approach
MeRT for Treatment of Concussions and Brain Injuries
MeRT® is an emerging technology that aims to improve brain function and communication. The equipment used is FDA-cleared to treat Major Depressive Disorder and OCD and is used off-label to treat a wide variety of conditions, including Traumatic Brain Injuries or Concussions.
Simply stated, we use magnetic fields to stimulate and balance brain function, guided by very sophisticated imaging and diagnostics.
Patients who have had Traumatic Brain Injuries (TBIs) or Concussions can experience after-effects well after the initial injury, and some may never fully recover. After the initial recovery, MeRT can be used to stimulate and assist the brain in improving connectivity and communication. In many cases, this has greatly improved recovery results.
See some of the RESEARCH STUDIES.
Call Our New Patient Coordinator to Learn More
(619) 255-2101
Or fill in the form below and she will contact you.
Listen to Jason O.’s Testimonial About How MeRT Helped Him Reclaim His Quality of Life After Suffering a TBI
46 Different Specialists, 29 Treatments, 40 Medications—Nothing Helped.
Then David Tried a NEW Treatment for his Traumatic Brain Injury.

For the next five years, he saw 46 different specialists: neurologists, psychologists, pain management specialists, orthopedic doctors, chiropractors, and physical therapists, which included 29 different treatments, from physical therapy to sensory deprivation tanks, meditation to biofeedback, and more. He was prescribed a multitude of different medications and supplements during these years and eventually ended up with a drug addiction problem as well.
While some of these approaches did help, he was still far from recovering his quality of life. Then he discovered MeRT, Magnetic e-Resonance Therapy.
“Everything changed when I started treatment. Within two weeks, I was sleeping better. I was off all 12 of the meds I was on when I began treatment, and I was starting to enjoy life again. After the first month, I was socializing with people again. I was able to work out for the first time in years, and I started to help my wife with the bills and our budget. As I write this, I just completed my sixth week of treatment. A conservative estimate is that I have had a 60–70% reduction of the symptoms I listed above and have a whole new lease on life.”
 Non-invasive and Drug-Free
Non-invasive and Drug-Free
What is MeRT?
MeRT stands for Magnetic Resonance Therapy. MeRT is a tailored, highly individualized form of TMS or Transcranial Magnetic Stimulation. In simpler terms, we use magnetic waves to stimulate specifically targeted areas of the brain that have been found to not be communicating or functioning optimally.
This is determined through sophisticated diagnostic tools and imaging, which are used to plan a tailored treatment approach just for you.
How Do I Know…
Is MeRT the Right Treatment?
We understand that MeRT is a relatively new treatment, and you may not be sure if this is right for your situation. However, know that this is not a decision you have to make right away or all alone.
Your first step is a simple phone consultation with our New Patient Coordinator. During this free, no-obligation consultation, you can discuss symptoms and history, ask all the questions you want, and have her explain the protocols and fees. She can also further explain the treatment itself.
After the call, if you are interested in taking the next step, we can set up an appointment for a qEEG (a simple, painless, and non-invasive brain scan).
EEG/EKG Testing
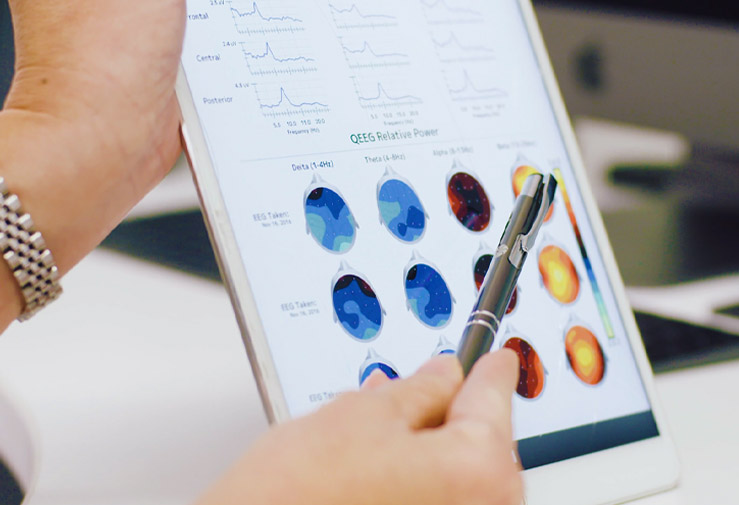
The qEEG/EKG testing is performed by our chief neurotechnician and takes approximately 45 minutes. However, if you are seeking treatment for your child with autism, please plan on spending an hour with us.
We will also gather your new patient paperwork at this time and get you scheduled for your initial assessment period of treatment.
Clinical Evaluation and Consultation
Your second appointment will be a clinical evaluation with Nurse Practitioner Kayleigh Prowse, which takes approximately 45 minutes. You can have this appointment via Telemedicine or in-clinic, whichever you prefer. Please note that if you choose a Telemedicine appointment and are seeking treatment for your child, your child will need to be present.
During this consultation, Kayleigh will answer all your questions and discuss your applicable treatment plan. You will also have an opportunity to meet with our physician and Medical Director, Julie Kim, M.D.
Assessment Period
Six weeks of treatment are recommended for patients undergoing MeRT to achieve optimal and long-lasting results. However, prior to committing to the six weeks, we have each patient go through an assessment period of treatment to see how they will respond. This assessment period is included in the six weeks of treatment.
The assessment is two weeks long. It consists of nine treatment sessions, followed by a repeat qEEG. Treatment would be provided the first week, Monday through Friday, and the following week, Monday through Thursday. A typical treatment session lasts about 30-45 minutes. Additionally, the follow-up qEEG results will be covered with you by your provider.
If clinical changes are occurring as they should, and the qEEG also shows progress, then you would then continue treatment, which would occur five days per week, Monday through Friday. Generally, you will begin to feel the benefits of treatment within a week or two, but because treatment is cumulative, should continue to note improvements throughout the course of your treatment, and even for some weeks after treatment. Because treatment is consecutive, you must be able to stay in or around the area while undergoing your therapy.
For those not ready to commit to an assessment period, or if we need to see the results of the testing to confirm that MeRT can help, we also offer the option of coming in for a qEEG/EKG and then having a consultation with Kayleigh or Dr. Kim to go over the results. After your clinical consultation, you will still have the option of going through an assessment period should you choose to do so.
Continuing Treatment
If clinical changes are occurring as they should and the qEEG also shows progress, you will then continue treatment. This ongoing treatment occurs five days per week, Monday through Friday. You should start to feel the benefits of treatment within a week or two, but because treatment is cumulative, you should continue to note improvements throughout the course of your treatment and even for some weeks afterward. Additionally, because we perform treatment on consecutive days, you must be able to stay in or around the San Diego area while undergoing your therapy.
Because each person’s brain and condition are unique, we customize treatment protocols specifically for each patient, guided by the qEEG results. Repeat qEEGs and clinical consultations occur every two weeks throughout treatment.
As a note, the potential side effects of treatment are minimal and should begin to dissipate as you progress through treatment. Moreover, the effects of treatment generally last a lifetime, though some patients prefer occasional follow-up treatment as needed.
Improvements and results of MeRT are based on strict and active observation of our treatment protocols. Results may vary based on each person and are not guaranteed.
Insurance Coverage and Payment Options
We are an in-network provider with TRICARE. If you have TRICARE insurance, it is possible that your policy may provide coverage for you or a family member, depending on your specific policy and condition. Our New Patient Coordinator can discuss this with you in further detail.
For all other insurance, we are considered out-of-network and cannot file insurance on your behalf. We can, however, provide you with the appropriate paperwork at the end of your treatment. Then, you can submit it to your insurance company to see if they will reimburse you.
Currently, rTMS is FDA-approved for Depression and OCD (Obsessive Compulsive Disorder.) Treatment for all other conditions is considered “off-label.” However, for non-FDA-approved treatment, it is not likely that insurance will provide reimbursement for our protocols.
Some patients have reported that they have been able to receive some reimbursement for EEGs or clinical evaluations. However, this depends on their health coverage. Additionally, Medicare patients have reported that their coverage provides no reimbursement for MeRT.
We take all major credit cards, including Visa, MasterCard, American Express, and Discover.
Care Credit
Care Credit is also an option to help finance medical expenses and is a separate company from The Brain Treatment Center San Diego. This is a credit card you can use to cover medical expenses and services. Additionally, they typically offer zero-interest financing for 12 months.
Usually, when you go to the Care Credit website and apply, they will rapidly let you know if you receive approval.
MeRT for TBI Treatment Featured on The Broken Brain Podcast

Dr. Eric Won from Wave Neuroscience (the parent company of MeRT treatment protocols) speaks about using MeRT with military members and veterans who have experienced TBIs, depression, and PTSD from serving their country. Dr. Won also gives shares some incredible successes after treatment.
Click here to watch this informative and fascinating episode.
MeRT’s Effectiveness in Treating Symptoms of Traumatic Brain Injury and Concussions
Targeted rTMS (repetitive transcranial magnetic stimulation) is a key element of our MeRT treatment for head injuries. Here are some of the many studies showing the effectiveness of rTMS:
The use of repetitive transcranial magnetic stimulation (rTMS) following traumatic brain injury (TBI): A scoping review
Evidence suggests that rTMS has the potential to be an efficacious therapeutic intervention for multiple symptoms after TBI, including depression, dizziness, central pain, and visual neglect. “
Neuromodulatory Interventions for Traumatic Brain Injury
In this special issue of the Journal of Head Trauma Rehabilitation, we share with readers some of the latest advancements in neuromodulation specific to TBI, while providing the framework to further our understanding of how and why functional skills are likely improved. While neuromodulatory interventions can play a critical role in functional recovery for those with TBI, the heterogenous nature of TBI means that clinical implementation of neuromodulation will require understanding, at the individual and group levels, of how, when, and where to alter brain activity to support sustained recovery of sensory and higher order functions.”
 The role of transcranial magnetic stimulation in treating depression after traumatic brain injury
The role of transcranial magnetic stimulation in treating depression after traumatic brain injury
This study suggests that rTMS is a potential treatment option for depression following TBI. Both 15 to 16 session and 30 to 38 session cohorts showed significant decreases in depression as measured by PHQ-9 following rTMS treatment. These findings support the use of rTMS in post-concussion depression treatment and highlight the need for more research on rTMS therapy following TBI.”
Randomized trial of rTMS in traumatic brain injury: improved subjective neurobehavioral symptoms and increases in EEG delta activity
Subjective measures of depression, sleep dysfunction, post-concussive symptoms (PCS), and executive function showed significant improvement with stimulation, retaining improved levels at two-week follow-up. EEG delta power exhibited elevation one week after stimulation cessation.”
Neural mechanisms of emotional health in traumatic brain injury patients undergoing rTMS treatment
Our findings uncover the neural mechanisms underlying the improvement in emotional well-being in TBI due to application of neuromodulation. The main effect of rTMS is to reduce emotional disorders and hence consequently it may improve cognitive and executive functions.”
Low frequency transcranial magnetic stimulation for cognitive recovery after traumatic brain injury: A case report
Our results are consistent with studies showing improved cognitive functioning in TBI following a unilateral or bilateral rTMS protocol that used low frequency rTMS over the right DLPFC. Therefore, this stimulation site may be promising for improving cognitive recovery in TBI, especially when combined with cognitive rehabilitation.”
Repetitive Transcranial Magnetic Stimulation for Treatment of Depression in a Patient With Severe Traumatic Brain Injury
Case Report: A 37-year-old male with history of anxiety and bipolar depression incurred a TBI after a 60-foot fall. After his physical recovery, the patient had refractory depression. Eight months after the TBI event, he underwent a 6-week course of rTMS treatment and had a 70.8% improvement in mood symptoms by the end of the therapy as indicated by the Patient Health Questionnaire-9, transitioning from severe to mild depression according to the scoring system. Clinical correlation during the months following conclusion of rTMS therapy showed no signs of remission or adverse side effects. The patient remains stable and lives independently 1 year after treatment with mood-stabilizing medications.
“Conclusion: This case provides evidence for successful treatment of refractory depressive symptoms after severe TBI with the addition of rTMS to psychotherapy and mood-stabilizing medications, supporting the safety and tolerability of this novel therapeutic approach. Further studies are needed to validate the contribution of rTMS for management of mood symptoms in patients with TBI.”
 Interested but not sure?
Interested but not sure?
Talk with our New Patient Coordinator
It’s normal for patients and their families affected by neurological conditions to feel frustrated and isolated. After all, many have lost hope that treatment can improve their condition. We understand what you may be going through.
However, there is hope. MeRT has helped patients restore their brain function, reclaim their lives, and feel passionate about living again. That’s why we want to help guide you through the process so that you can make an informed decision about whether MeRT is the right treatment for you or your child.
It costs nothing to call us and talk about what is happening. Our New Patient Coordinator is here for you. She understands your pain and can answer all your questions. Additionally, she can explain the process and protocols, costs, possible insurance benefits, and any other details you want to know. During this no-obligation consultation, she will take all the time you need to know whether you should take the next steps.
Call Our New Patient Coordinator to Learn More
(619) 255-2101
Or fill in the form below and she will contact you.
Contact Us
For more information or to speak with our New Patient Coordinator, please fill in the information below.

 Symptoms of a Concussion or Traumatic Brain Injury
Symptoms of a Concussion or Traumatic Brain Injury An Entirely New Approach
An Entirely New Approach Non-invasive and Drug-Free
Non-invasive and Drug-Free

 Interested but not sure?
Interested but not sure?